|
| Image 1: This little bugger obviously has too little inflammation going on ;-) |
Are you "on fire"? Inflammation has been implicated as the root cause of almost all modern disease: obesity, diabetes, heart disease, cancer, you name it. Soothing the flames via natural and supplemental anti-oxidants has thusly been proposed and marketed as a solution for many of the aforementioned health problems.
Yet,
despite tons of vitamins, anti-oxidants and all the other "healthy" stuff we are taking and consuming on a daily basis, the number of morbidly obese people, diabetics and heart attack patients appears to be ever-increasing... how can that be?
A possible answer to that question comes from scientists from the
Saha Cardiovascular Research Center at the
University of Kentucky College of Medicine in Lexington, Kentucky, US (
Findeisen. 2011) -
we simply got everything wrong! The observation that insulin resistance and beta-cell dysfunction usually occur in the presence of large amounts so-called reactive oxygen specimen (ROS) lead scientists to propose that there was a causative relationship between these two events, of which the data only shows that they are corollary.
 |
| Image 2: Whenever there is a fire, the firefighters are not far away, but does this correlation indicate that all firefighters are firebugs? (img texarkanagazette.com) |
Despite the fact that the d
istinction between correlation and causation should be obvious, correlations have a long history of being mistaken as causative factors in the history of science. The corollary elevation of total cholesterol in heart disease patients, for example, is the reason that millions of well-educated people world-wide still believe that cholesterol would cause heart disease - an erroneous conclusion for which my friend,
Carl Lenore, has coined a very fitting analogy (actually the analogy spans all those "corollary causation"): When there is
a fire in down-town New York, it won't take long until the place is packed with firefighters, nevertheless, no sane observer would get the idea that the corollary appearance of firefighters on the scene would be the reason for the fire.
Here, at the SuppVersity, you have already learned that a group of researchers from Germany has invested a lot of work into research on the
beneficial effects of inflammation (
Ristow. 2010). Now, with the data from Hannes M. Findeisen (who unquestionably is a German or has German ancestors, as well ;-) et al., evidence begins to accumulate that the role of reactive oxygen specimen in glucose homeostasis could in fact be a
beneficial and not a detrimental one. After all, Findeisen and his colleagues were able to show that the pharmacological
depletion of glutathion, our natural broadband fire-extinguisher, made mice
resistant to diet-induced obesity, increased energy expenditure and enhanced insulin sensitivity.
If you have listened to all the installments of the
Amino Acids for Super Humans Series on Carl Lenore's
Super Human Radio, you will already have heard me mention that
a methionine/cysteine-free diet has been shown years ago to have profound fat-burning, or I should say, weight-reducing effects on mice - no wonder, with methionine and cysteine being essential substrates for mammalian gluthation production, a lack of these dietary sulfur-amino acids induced a similar glutathion depletion as the
addition of 30mmol/l BSO to the drinking water of the mice in the Findeisen study (for more on the glutathion depleting effects of BSO, cf. Skapek. 1998; Mira. 2002; Cattan. 2008)
Even before the works of Ristow et al. and now Findeisen et al., it has been well-established that
reactive oxygen specimen, the purported villains of the 21st century, enhance cellular signaling (
Veal. 2007). About a year ago, Chang and Chang reported that H2O2, in particular, is a potent activator of protein signaling pathways, including insulin signaling and can even mimic insulin's effects by the inhibition of oxidation-sensitive protein tyrosinases (
Chang. 2010). With glutathion being the primary H2O2 scavenger in mammalian tissue, it is thus not surprising that
the BSO treated and thusly glutathion depleted mice in the Findeisen study displayed a more favorable response to a glucose tolerance test after 6 weeks of treatment with BSO and a 45%(high)-fat diet (cf. figure 1).
 |
| Figure 1: Glucose levels in mg/dl after oral glucose tolerance test in mice after 6 weeks on a high-fat diet (47% fat) with or without 30mmol/L BSO in their drinking water (data adapted from Findeisen. 2011) |
These results are surprising, also because the
daily food and water intake of the mice was identical. The latter cannot be said of their calorie-expenditure, daily activity level (cf. figure 2) and the activity of the "fat burning" uncoupling protein UCP2 (+100%), the elevation of which increases thermogenesis and energy expenditure.
 |
| Figure 2: Relative changes in energy expenditure and daily activity due to BSO induced glutathion depletion in mice on a high fat diet compared to non-treated control (data calculated based on Findeisen. 2011) |
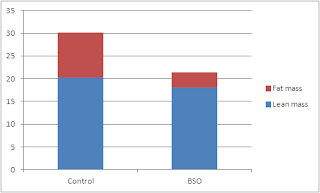
Now, most importantly for you, as a physical culturist, may be that glutathione depleted mice did not simply fail to thrive or shrivel away - they were, as Findeisen points out...
completely protected from diet-induced obesity, despite similar food intake and water consumption. Analysis of body composition in mice fed a HFD diet confirmed significantly decreased fat mass in BSO-treated mice without significant differences in lean body mass, indicating that the difference in body weight was due to reduced fat mass in BSO-treated mice.
If you don't believe the words, I suggest you take a look at the data in figure 3 - while the control mice had a body fat percentage of whopping 32% the mice on BSO with their ~16% body fat were well within the normal range for lab-mice.
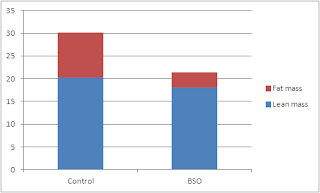 |
| Figure 3: Fat and lean mass (in g) of mice from the control group and the glutathion-depleted group after 6 weeks on a hypercaloric high fat diet (data adapted from Findeisen. 2011) |
Even the researchers appeared to be surprised by the profound effects glutathion depletion had on the rodent's ability to accumulate body fat. As far as the
underlying reasons are concerned, they speculate that it was ...
[...] possible that the observed increase in the expression of UCP-2 and UCP-3 in BSO-treated mice induced mitochondrial uncoupling [...] Alternatively, the enhanced energy expenditure in BSO-treated mice might be the result of increased locomotor activity. In skeletal muscle, ROS are necessary for optimal contractile function, force production, and exercise-induced adaptations. Furthermore, particularly H2O2 is increasingly recognized as
a potent neuromodulator. It is therefore conceivable, that glutathione depletion may lead to activity-stimulating changes in the redox environment of muscle or brain.
Now, it is however questionable in how far any of these three phenomena would occur in human beings, as well. While the
lack of large amounts of UCP-sensitive brown adipose tissue would decrease the UCP induced thermogenic response to glutathione depletion,
locomotor activity is something that appears to be completely blocked in the modern couch potato, anyways. It would thus warrant further research (and studies into the general
safety of this approach) before it would appear warranted that you take a spoon of BSO with every meal to counter the negative effects of your last binge ;-)