 |
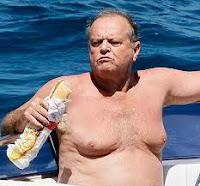
| Image 1: Is it what he eats, is it what he drinks or is it just andropause? Whatever it may be, Jack does not have the "classic gyno". |
If it's benign you got to live with it!
The idea, "if it's not cancerous", it won't hurt, is probably also the main reason for the lack of viable (N=5), let alone "proven" (N=1, surgery) treatment strategies. A couple of case-reports and small scale studies do yet suggest that its surgical removal, which is uncertainly the method of choice for non-benign or exuberantly proliferating tissue growth, is not the only option you may have to get rid of a condition of which I suspect that it has been bothering many of you for years now.
Whichever of the following strategies you may pick, your first step should always be to avoid / drop all of the 45+ offenders I mentioned in the last installment, and to avoid the 10 previously discussed anti-androgens like a plague. Yet while these "passive" treatments may suffice to stop your breasts from growing even further, it is unlikely that they will put a long lasting real gyno (not just normal fat!) in remission. If you are among these unfortunate, yet certainly not rare cases, you may have to resort to one or more of the following "alternative" (from the perspective of most MDs) but not mutual exclusive anti-gyno strategies.
Getting rid of "gyno" by losing body fat (not weight!)
 |
| Image 2: This poor boy may not know it, but he is just lying the fat foundation for embarrassing female breasts |
Puberty and the spontaneous regression of pubertal gynecomastia can yet also serve as an encouraging example that an ample increase and stabilization in the androgen to estrogen ratio, as it should occur towards the end of puberty, can send mild cases of pubertal gynecomastia and lipomastia into remission. Similar effects can be seen in adults, when
- you lose fat without starving yourself - Starvation would lead to decreased androgen production and could, if anything, help not to make things even worse; more often than not, it does yet make things worse. After all, large breasts on a skinny man look even worse than breasts of the same size on a slightly chubby guy.
- you are gradually losing fat over a long period of time - It is more than likely that the chest fat is going to be the last to go; in fact, it may take a profound reduction in total body fat shift the androgen-to-estrogen ration into the normal range before you see any improvements
- you don't resort to questionable fat burners - with herbs, tea or whatever extracts in them that will have either direct estrogenic or anti-androgenic side-effects or mess with the cytochrome P450 cascade of your liver (see previous installment)
Getting rid of "gyno" with Tomaxifen, a selective estrogen receptor inhibitor
In view of its kinship with breast cancer, it should not surprise you that the single scientifically well-established anti-gyno agent is a selective estrogen receptor modulator, in short SERM. Tamoxifen, brand name Nolvadex, has been used in a couple of small scale trial with reasonable success (e.g. Parker. 1986; Algaratnam. 1987; McDermontt. 1990; Ting. 2000), the results of which Braunstein et al. summarize as follows (Braunstein. 2007):
[A]dministered orally at a dose of 20 mg daily for up to 3 months, has been shown to be effective in randomized and nonrandom-ized trials, resulting in partial regression of gynecomastia in approximately 80% of patients and complete regression in about 60%.Despite the existent evidence that would support the use of Tamoxifen as the "anti-gyno" drug of choice, Daughty and Wilson, in their 2003 letter to the editor of the British Journal of Medicine, rightly state:
The evidence base for their conclusion is small (135 patients) and is certainly not derived from randomised controlled clinical trials. [...] until more evidence shows that tamoxifen is safe in this condition it should not be recommended as first line treatment, especially in pubertal boys.If you add to that the potential hepatoxicity (cf. "Milk Thistle Against Tamoxifen Induced Liver Injury"), as well as the two documented cases of epigastric distress and the one known case of post-traumatic deep-vein thrombois, it is self evident that you and your medical practitioner should carefully monitor your liver as well as other health parameters if you decide to give Tamoxifen or alternatively Clomiphene (cf. Plourde. 1983) a try.
Getting rid of "gyno" with aromatase inhibotors
There is also some evidence from case reports that would support the use of 2nd generation aromatase inhibitors (AI), Letrozole, in particular, to combat gynecomastia. As Braunstein et al. point out (Braunstein. 2007), their efficiency seems yet to be limited to cases, where over-aromatization of testosterone into estrogen is the underlying reason of the the problem. If this applies to you, talk to your medical practitioner about the use of a very low dose of letrozole, like 2x per week 2.5mg, or resort to 25mg of the (in the US formerly) OTC, yet very potent aromatase inhibitor ATD (more is counter-indicated because it could start "clogging" your androgen receptor, cf. "Antiandrogen effects of ATD").
Note: In a 2004 randomized controlled trial by Plourde et al. the "standard AI", Anastrazol, was ineffective for patients with residual pubertal gynecomastia (Plourde. 2004). Similarly, Riepe et al. found no effects in pubertal boys other than a reduction in breast tenderness (Riepe. 2004). It is therefore, as Sarah L. Maidment points out not not just that "Anastrozole may not be more effective than placebo in decreasing the size or volume of breast tissue in persistent pubertal gynaecomastia", but also that "its long-term effects and safety are still unknown" (Maidment. 2010).
If the over-aromatization is related to an increased amount of body fat, this treatment strategy should be complemented by appropriate lifestyle changes (diet + exercise; follow the SuppVersity for daily tips on what works). The effectiveness of your weight loss efforts will be largely augmented by the restoration of a normal estrogen-to-androgen ratio and will hopefully allow you to maintain the latter once you seize taking the drug.Update: If you hesitate to use a "real" aromatase inhibitor you could also resort to melatonin (kudos to Peter Rouse for the reminder), of which a dose as low as 3mg melatonin per day taken at 5pm for 6-month can shift the testosterone-to-estrogen ratio into the desired direction (Luboshitzky. 2002)
Getting rid of "gyno" with topical DHT cream
Largely unknown in the US, but a relatively common treatment strategy in Europe, in particular in France, is the use of topical DHT cream. The available literature on this issue is scarce. The results of one of the few well-documented trials by Kuhn et al. are yet promising and stand in line with the natural "anti-estrogenic" effects of dihydrotestosterone (Kuhn. 1983):
Local administration of DHT was followed by the complete disappearance of gynaecomastia in 10 patients, partial regression in 19 and no change in 11 patients after 4 to 20 weeks of percutaneous DHT (125 mg twice daily).This is a 33% success rate in patients with idiopathic (meaning we don't know the underlying reason) gynecomastia. That is less effective than tamoxifen and certainly neither what you would call a "tried and proven" method, but probably better than the bro-scientific use of DHT-precursors and pro-steroids with structural resemblance to DHT. Especially in the US, it may however difficult to find a medical practitioner who would be willing to prescribe and monitor this treatment, I guess.
Conclusion and the last resort: Surgery
In case none of the pharmacological approaches works, you can still resort to to surgery (or radio-therapy, but I guess most of you will prefer the knife, right?), the "gold standard therapy for symptomatic gynecomastia in most patients" (Johson. 2011). Just make sure you do not spoil the ship for a ha'porth of tar - or put more simply, go and seek an expert!
