There is al-wheys something new about whey ;-)
As the researchers point out the beneficial effects of whey proteins don't just go way beyond their muscle building effects and are mediated by several and not just one of it's amino acid, protein and peptide ingredients:
"Whey proteins (WP), a by-product of the cheese-making industry, possess nutritional benefits as a source of protein of high biological value. Whey products and whey-derived peptides have demonstrated a number of anti-inflammatory effects. These anti-inflammatory effects include decreased cytokine release in rodent models of ischaemia– reperfusion and exposure to LPS. In addition, individual whey constituents, such as lactoferrin or glycomacropeptide, and peptides released from these by pepsin– pancreatin hydrolysis exhibit anti-inflammatory effects, such as suppression of tissue neutrophilia or inhibition of inflammatory cytokine release." (Iskandar. 2013)In that, whey proteins have been shown to be particularly useful for the treatment and/or management of chronic inflammatory diseases such as cystic fibrosis, a disease passed down through families that causes thick, sticky mucus to build up in the lungs, digestive tract, and other areas of the body and a disease that will probably make you - just like me - think about the high cysteine content of whey, immediately.
"Under pressure..."
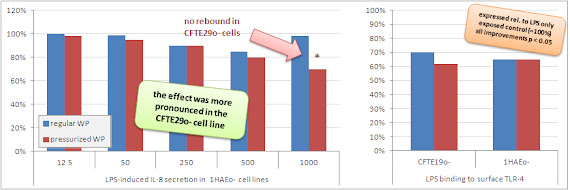
For the study at hand the researchers used two different epithelial cell types and added lipopsaccharides (LPS), as well as
- regular whey (Inpro 90 Whey Protein Isolate from Vitalus Nutrition) that had been enzymatically hydrolysated (=predigested) to yield a product that would be similar to what many supplement are now selling you as either intra- or post-workout "super whey" (their not my claim ;-), or
- pressurized whey, which was based on the same raw material, but was pressurized before being hydrolysated
A similar difference was observed in the results FRAP essay (FRAB stands for ferric reducing ability of plasma and the results provide information about the general antioxidant defenses of the cells). While the CFTE29o- cells (shown in figure 2) were happy with both whey protein hydrolysate, the pressurized WPH had a minimal, but statistically non-significant edge in the 1HAEOo- cells.
Is there anything special about pressurized hydrolysates?
In previous studies the researchers had already established that pressurization of WP improves its
in vitro digestibility, promotes the release of novel peptides by gastrointestinal digestive enzymes and enhances the antiinflammatory effect (Vilela. 2006).
"These in vitro findings were also confirmed in clinical studies. Thus, a 2-week supplementation with pressurised whey increased the levels of glutathione, a crucial low-molecular anantioxidant, in peripheral blood mononuclear cel. Further, we have reported that a 1-month dietary supplementation with pressurised whey improved nutritional status and markers of systemic inflammation in patients with CF [cystic fibrosis]." (Iskandar. 2012)In the study at hand, the research team from Canada did now want to (a) investigate the potential anti-inflammatory and antioxidant effects of pressurized and regular whey protein hydrolysates in the context of cystic fibrosis and non- CF respiratory epithelial cells and (b) explore the mechanisms by which pressurised and native whey exert their beneficial anti-inflammatory effects. Their research hypothesis was that it is the difference in peptide (=complex bond of amino acids that has different effects from the same amino acids in isolation) availability that is enhanced by the pressurisation of whey that's responsible for it's superiority compared to regular whey proteins.
Establishing the (leaky) gut, bacteria, non-alcoholic fatty liver disease connection
With the researchers focus being on cystic fibrosis, the results of this in-vitro trial are still highly meaningful for all of us. In particular the more potent increase in overall anti-oxidant capacity upon exposure of the epithelial cell lines would suggest that the ingestion of pressurized whey proteins could exert similar benficial effects in other parts of the body, specifically the digestive tract, as well.
 |
| Suggested read: "Plus: 20+ Things to Protect and Restore the Integrity of Your Intestinal Wall" (read more) |
Bottom line: So will just having your daily whey protect your gut from all assaults? Probably not, but is may be just another one of the many small things which may not render your intestinal wall and overall immune system bullet-proof but will at least help them to come with the omnipresent and 24/7 assault they are exposed to. Whether it's really got to be pressurized whey, on the other hand, remains questionable. Personally, I don't think so - if you take a look at the dose-dependently reduced expression of IL-8 in response to LPS exposure upon co-administration with pressurized and normal whey, it seems as if the pressurized variety did not only have the edge, but was also lacking the rebound effect that occurred at very high doses in the 1HAEo-cells.
 |
| If you want to live out your OCD tendencies on your whey intake, start with rule #1 "Never Sip Your Whey" (read why). |
References:
- Iskandar MM, Dauletbaev N, Kubow S, Mawji N, Lands LC. Whey protein hydrolysates decrease IL-8 secretion in lipopolysaccharide (LPS)-stimulated respiratory epithelial cells by affecting LPS binding to Toll-like receptor 4. Br J Nutr. 2013 Jan 3:1-11.
- Frasinariu OE, Ceccarelli S, Alisi A, Moraru E, Nobili V. Gut-liver axis and fibrosis in nonalcoholic fatty liver disease: An input for novel therapies. Dig Liver Dis. 2012 Dec 29.
- Vilela RM, Lands LC, Chan HM, Azadi B, Kubow S. High hydrostatic pressure enhances whey protein digestibility to generate whey peptides that improve glutathione status in CFTR-deficient lung epithelial cells. Mol Nutr Food Res. 2006 Nov;50(11):1013-29.